What is nutrition? 6,7

Nutrition is the act or process of nourishing or being nourished. Research has indicated that proper nutrition in Duchenne muscular dystrophy is one component that can improve the overall quality of life.
While there are several considerations regarding caloric consumption, including physical activity, capability of ambulation, and steroid use, specialists in the field suggest that daily caloric consumption should be 80% of what individuals without Duchenne muscular dystrophy consume. Avoidance of excessive calories, salt (no more than 1500 mg daily), and adequate calcium intake are recommended.
Scheduling a regular visit with a registered dietician nutritionist (RDN) can help you ensure that you or your child is getting the proper nutrition they need without gaining excessive amounts of weight due to steroid use and lessened activity levels. A gastroenterologist can also help with issues such as constipation and a speech-language pathologist for difficulty swallowing.
Keep in mind, it’s never too late to start! Meal planning is often an effective means with which to involve all members of the family. Engage support from your healthcare team, including a registered dietitian nutritionist or registered dietitian to develop a plan customized for proper nutrition with Duchenne.
7 Daily Points to consider for nutrition in Duchenne 6
- Start off the day with a protein rich breakfast. AVOID sweets and sugary based food by consuming foods that contain less than 9g sugar/serving
- Increase water intake. Amount of daily water needs is equal to ½ your body weight i.e. for a person weighing 60 pounds, his minimum water intake should be 30 oz.
- AVOID foods high in sodium. Don’t add salt and use low sodium food products
- Grill, bake, & broil proteins. Use lean fish and poultry.
- Include a salad at lunch and dinner
- Eat less starchy foods – replace with less starchy vegetables
- AVOID Constipation by consuming adequate water and increasing fiber consumption
Water 8

Adequate water intake helps to eliminate waste from the body, maintain a normal body temperature, lubricate joints, and maintain healthy tissue. The general guideline for the consumption of water in ounces (10 oz. = 1 glass of water) is your weight divided by two.
Example: 200 lb / 2 = 100 oz of water daily
Proteins

You should aim for 1.5 grams of protein per kilogram of body weight.8 Protein is an important part of any diet, especially in Duchenne, and can help you feel fuller for longer so you don’t need to supplement with unhealthy snacks.
The most common way to satisfy your protein requirements is through lean meat, like chicken, grass fed beef, and lamb, and fish. However, you can also get the proper amount through beans, yogurt, and nuts.
Carbs

Carbs, or carbohydrates, are found in much of what we eat, including starches (pasta, grain, and potatoes), dairy (yogurt, cheese, and milk), fruit (bananas, oranges, and grapes), and veggies (cabbage, carrots, and bell peppers), and processed food (cookies, candy bars, chips).
That can further be divided into high glycemic foods, or those that the body breaks down quickly, and low glycemic foods; those that the body breaks down slowly. It is ideal to choose foods with lower glycemic indexes so we maintain our energy over the day. So instead of having potato chips for a snack, go for an apple.
List of low glycemic foods12
- Vegetables: Peppers, broccoli, tomatoes, lettuce and eggplants.
- Fruits: Strawberries, apples, lemons, limes and pears.
- Legumes: Chickpeas, beans (dried or boiled) and legumes.
- Dairy: Whole/full-fat milk and plain yogurt.
- Sweets: Dark chocolate with more than 70% cocoa.
- Nuts: Cashews and peanuts.
Fats

Healthy fats are found in foods like salmon, avocado, olive oil, and meat. Try to include monounsaturated fats and polyunsaturated fats in your diet with Duchenne instead of saturated fats where possible.
Monounsaturated fats
- Olive oil
- Sunflower oil
- Fish oil
Polyunsaturated fats
- Soybean oil
- Corn oil
- Safflower oil
Saturated fats
- Animal products
- Processed food (Oreos, potato chips, candy bar, etc.)
Fiber
Take a look at the following handout from the University of Virginia, which tells us why fiber is so important to nutrition in Duchenne and how we can get enough of it in our diet.
Minerals

Minerals such as calcium, magnesium, and zinc can activate thousands of enzymatic reactions, assist with vitamin functions, help metabolize carbs, proteins, and fats, and regulate water balance. It’s an important part of nutrition for Duchenne. More than 3,800 minerals have been identified by scientists.8 It is recommended to take a daily multivitamin that includes mineral supplements. Examples include chewable tablets such as Flintstones for young boys and men’s multi-vitamins for teens.
Vitamins & supplements5
Daily calcium needs are based on actual intake. The first step is to collect information on what intake is obtained from food and then determine if it is sufficient. When under the ideal amount, supplements can be added. It is important to determine the actual calcium intake from food and then decide if additional calcium is needed. A body can get TOO much calcium so it is imperative to work with your health care team to determine a plan best tailored to your child’s needs.
Calcium needs for Males8
| Age | Adequate Intake (mg/day) | Steroids w/ DMD (mg/day) |
| 1-3 | 500 | 750 |
| 4-8 | 800 | 1200 |
| 9-18 | 1300 | 1500 |
| 19-70 | 1000 | 1500 |
Nutrition in Duchenne breakdown8
| Proteins | Fats | Carbohydrates | Fiber | Water | Vitamin D |
| 10-35% (of calories) | 30-40% | 45-65% | 25-30 grams/day | 1 oz/2lb/day | 1,000-4,000 units |
Sample Meal Plans8
Determine how many calories you need on a daily basis with the MyPlate.Gov widget below. Click the link to see the best plan for your caloric needs.
Quick healthy snacks:
- Yogurt
- String cheese
- Low-fat microwave popcorn
- Canned fruit or applesauce in single-serving containers
- Raisins and other dried fruit
- Whole wheat crackers
- Pretzels
- Flavored rice cakes
- Unsalted nuts
- Baby carrots
- Cherry tomatoes
Additional Resources
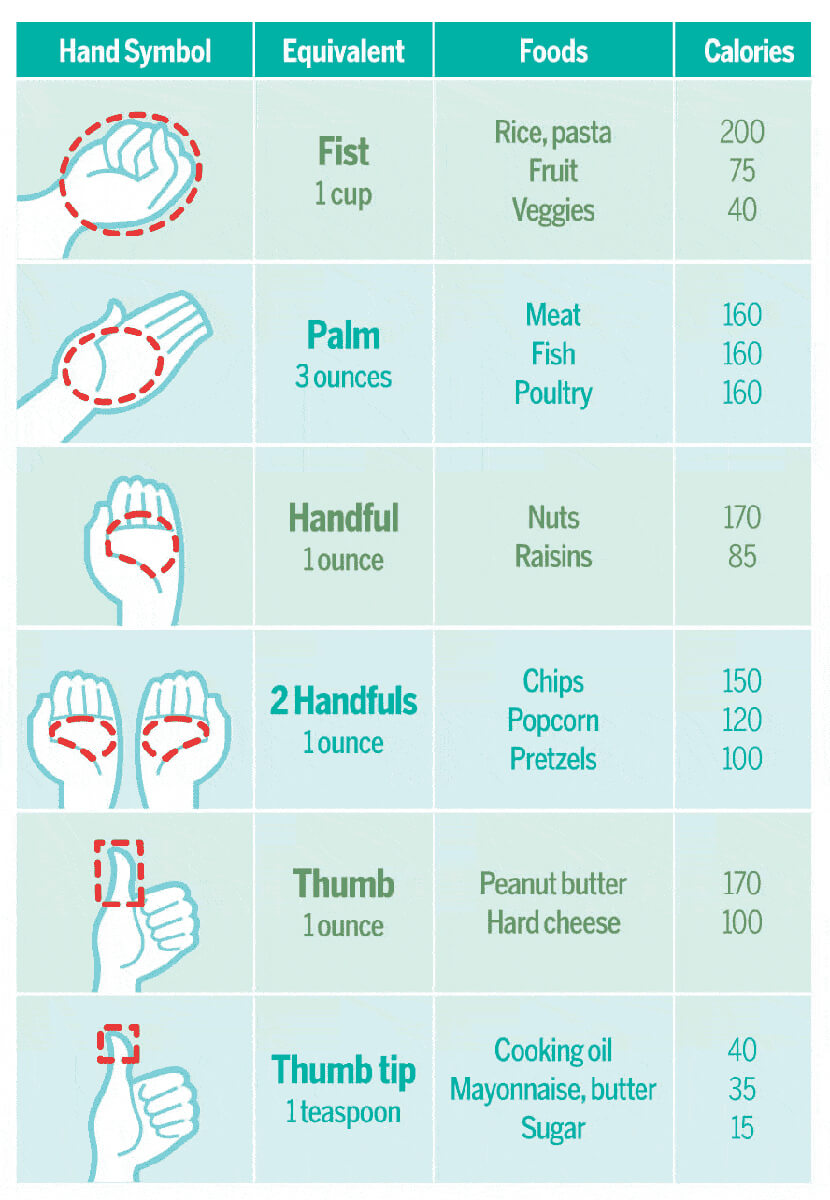
Portions3
Oftentimes, we think we need more food than is necessary. This graphic can help you think about what your portions should look like.
Food intake record5
A food intake record can help you determine what you require in your diet. Ask your nutritionist about completing one yourself. These details below should be completed following a three-day food intake record in collaboration with your child’s dietitian.
| Type | Amount | Units |
| Calories | Calories/day | |
| Protein | Grams/day | |
| Fluids | Ounces/day | |
| Calcium | Milligrams/day | |
| *Additional Calcium supplement | *when indicated | |
| Vitamin D3 | 1,000-4,000 | International units/day |
| Sodium | 1,500 | Milligrams/day |
| Multivitamin/Mineral | 1 per day | Suggested Brand(s): Flintstones Complete Centrum Liquid Centrum Complete |
| *Other supplements | *when indicated |
Low FODMAP Diet 9
FODMAPs are a group of carbohydrates which are difficult for people with a slow moving gut to digest. To attain proper nutrition in Duchenne, it’s important to limit these kind of foods.
What does that stand for?
- Fermentable
- Oligosaccharides (oligo –“few,” saccharide – “sugar”)
- Disaccharides (“two sugars”)
- Monosaccharides (“one sugar”)
- And
- Polyols (these are sugar alcohols)
Symptoms of FODMAP intolerance include gas, abdominal discomfort, distention, bloating, fullness, nausea, and/or pain after eating foods containing FODMAPs.
Look out for the following FODMAPs on the ingredients list of the foods you typically buy.

- Fructose
- Lactose
- Fructooligosaccharides
- Galactooligosaccharides
- Sorbitol
- Mannitol
- Xylitol
- Maltitol
Foods that do not contain carbohydrates are not a concern. This includes meat, poultry, fish, eggs, butter, oils, and hard cheeses.
Over nutrition and under nutrition in patients with neuromuscular diseases 8
Decreased caloric needs, decreased resting energy expenditure, decreased physical activity, increased appetite due to medication, and lack of caloric restriction can all cause over nutrition in Duchenne. You can offset the risk of over nutrition with these suggestions below from Simona Salera, et al.
- Evaluate glucose metabolism; follow a low glycemic index diet
- Dietary control with the assistance of advice/support from a dietitian
- Limit caloric intake
- Reduce consumption of sugar-containing beverages
- Increase consumption of fruits and vegetables
- Limit the addition of oils and fats
- Use of behavior management techniques i.e. eat slowly and recognize satiety cues
You should also pay attention to the signs of undernutrition listed below so you or your child is receiving enough to eat as well.
- Decreased muscle strength
- Dysphagia/Swallowing difficulties
- Gastrointestinal problems (constipation, delayed gastric emptying)
- Prolonged mealtime
- Dependent feeding
- Increased energy requirements because of respiratory failure
Further reading8
- Gloss D, Moxley RT 3rd, Ashwal S, Oskoui M. Practice guideline update summary: Corticosteroid treatment of Duchenne muscular dystrophy: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016;86(5):465-472. doi:10.1212/WNL.0000000000002337
- Medical professionals and experts in the field believe a guide helps families understand the different stages of the disease. Please remember that some of the items in this guide won’t apply to your child or might apply at different times. Always know that you can contact your provider or the network of families and resources through the national nonprofits supporting this disease.
- Bushby K, et al. The Diagnosis and Management of Duchenne Muscular Dystrophy, part 1: diagnosis, and pharmacological and psychosocial management, Lancet Neurology 2010, 9(1) 77-93.
- Duchenne muscular dystrophy (DMD) is a severe, progressive disease that affects 1 in 3600–6000 live male births. The DMD Care Considerations Working Group was formed to evaluate assessments and interventions used in the management of diagnostics, gastroenterology and nutrition, rehabilitation, and neuromuscular, psychosocial, cardiovascular, respiratory, orthopedic, and surgical aspects of DMD. Through this group came two sets of guidelines for practitioners.
- Part 1 describes the methods used to generate the recommendations and the overall perspective on care, medications needed, and physical and mental health issues that arise.
- Bushby K, et al. The Diagnosis and Management of Duchenne Muscular Dystrophy, part 2: implementation of multidisciplinary care, Lancet Neurology 2010, 9(2) 177-189.
- Part 2 describes the prevention and management of symptoms and issues as they come about. Educating ourselves and knowing what the process will entail helps to manage symptoms, improve the quality of life, and increase longevity. A care plan helps with the management of rehabilitation, orthopedic (bone and spine), respiratory (lung), cardiovascular (heart), gastroenterology/nutrition (belly and food), and pain issues, as well as general surgical and emergency-room precautions.
Citations
- Bushby K, et al. (2009). Diagnosis and management of Duchenne muscular dystrophy, part 1: implementation of multidisciplinary care. The Lancet Neurology, 73-93.
- Bushby, K. et al. (2009). Diagnosis and management of Duchenne muscular dystrophy, part 2: implementation of multidisciplinary care. The Lancet Neurology, 177-189.
- Estimate Serving Sizes With Household Objects (Or Your Hands…). (2012, February 7). Retrieved from TopsyTasty: https://topsytasty.com
- Fawcett, Ph.D., RD, LD, K. (n.d.).
- From The Diagnosis and Management of Duchenne Muscular Dystrophy : A Guide for Families. (2010).
- Gloss, D., Moxley, R. T., Ashwal, S., & Oskoui, M. (2016). Practice guideline update summary: Corticosteroid treatment of Duchenne muscular dystrophy. Neurology, 465–472.
- Godshall, LD, CCHMC, B. (n.d.).
- Ramos-Platt, Neurologist, L. (n.d.).
- Simona, S., Francesca, M., Maurizio, M., Sophie, G., Sciacco, M., & Susanna, E. (2017). Nutritional Challenges in Duchenne Muscular Dystrophy. Nutrients.
- University of Virginia Health System: Digestive Health Center. (2014, October). Low FODMAP Diet. Retrieved from www.GInutrition.virginia.edu
- University of Virginia Health System: Digestive Health Center. (2015, October). High Fiber. Retrieved from www.GInutrition.virginia.edu
- What is the Glycemic Index? (2021, October 21) Retrieved from Mayo Clinic: https://health.clevelandclinic.org/glycemic-index/
Please be advised that the contents within the CureDuchenne site include a compilation of articles, advisements, and references from the community. The intent of this shared content is to serve as a point of reference for informational purposes. Please refer to your health care provider(s) for your individualized, specific care management needs.
The CureDuchenne website may contain links to external websites that are not provided and/or maintained by or in any way affiliated with CureDuchenne. Please note that CureDuchenne does not guarantee the accuracy, relevance, timeliness, or completeness of any information on these external websites.
